A Closer Look at Common Medical Billing Errors
Posted on July 31st, 2023 / Under Medical Billing / With No Comments
Medical billers and coders deal with thousands of codes when documenting procedures and other relevant treatments provided to patients, making medical billing errors inevitable in some cases. However, when these errors occur, they can impact the claims process, leading to denied claims or delayed reimbursement, resulting in a loss of revenue.
Typically, errors in medical billing occur due to basic mistakes made during the entire billing process, such as miscoding or misreporting. Understanding the reasons behind the most common medical billing errors can help minimize them, optimize the revenue cycle, and keep your patients satisfied.
Common Medical Billing Errors:
Duplicate Billing:
Duplicate billing is a common medical billing error that occurs when a patient gets billed more than once for the same procedure. This type of billing can be a mistake or can be done intentionally, which is also known as medical billing fraud.
For instance, if you have to repeat a procedure on the same day and there is a modifier misuse, such as not using modifier 76 in the bill, it will result in a duplicate billing mistake. Frequent duplicate billing can lead to rejected claims and negatively impact the facility’s reputation.
Undercoding:
Undercoding is another common error in medical billing, resulting in the codes added to the bill not fully reflecting the extent of services provided to the patient. The National Correct Coding Initiative necessitates that physicians must always use the CPT/HCPCS codes that accurately describe the services rendered rather than reporting less comprehensive codes.
This error typically occurs due to miscoding or if the provider is trying to avoid a denial or an audit. It’s crucial to prevent underbilling a patient in any situation, even if done as a sympathetic act towards a financially struggling patient, as it can lead to fraud charges and revenue loss.
Unbundling:
Unbundling is when a provider does not use a comprehensive code to bill a single procedure and instead uses separate CPT codes for it, resulting in overbilling the patient. Medical billing errors such as unbundling can be tricky to identify. If fragmenting billing codes is done intentionally to increase reimbursements from Medicaid or Medicare, it would be considered fraud and lead to legal repercussions.
Missed Deadlines:
Most insurance companies have strict deadlines for filing a claim, and some deadlines can be as stringent as 30 days. There can also be a limited timeline to follow up with claims and correct any billing errors. If a claim is denied because it was not filed on time, it can make the process of appealing the denial more complicated. To expedite the reimbursement process, ensure that you do not miss the deadline for filing medical claims.
Insurance Verification Issues:
One of the biggest reasons most medical claims are denied is insurance verification issues. This issue often stems from overreliance on pre-existing information and routine.
For example, suppose a patient frequently visits a facility to acquire treatment. In that case, the providers or staff can presume that their insurance information has not changed and fail to verify their eligibility. This can cause multiple issues, including the Coordination of Benefits (COB) error, which occurs when the patient has more than one insurance provider.
Missing or Incorrect Documentation:
Even the most basic errors, such as spelling mistakes or adding the wrong patient ID number into the medical billing software, can leave you with correcting patient information and resubmitting claims after denials. Missing or incorrect information, such as patient, provider, or insurance information, is one of the most common medical billing errors.
Ways to Prevent Medical Billing Errors:
Here are some ways you can prevent errors in medical billing:
- Update Your Practice’s Fee Schedule: Working on the existing fee schedule can cause your practice to suffer revenue loss, as reimbursement rates may vary when working with different insurance providers. Update the fee schedule to avoid any discrepancies.
- Implement EDI: Implementing electronic data interchange (EDI) will streamline the billing process by reducing the amount of time it takes a bill to be processed and improving accuracy in medical billing.
- Accounts Receivable Analysis: Accounts Receivable (AR) analysis will help you recover any overdue payments and conduct follow-up procedures to resolve denied claims.
- Double-Check Forms Before Filing Claims: Double-checking all forms to ensure the patient, insurance, and provider information is correct before you proceed to file a claim can save you from the headache of dealing with delayed payments and denied claims.
- Medical Billing Audits: Compliance issues and fraudulent claims can be avoided through medical billing audits. It will also improve collaboration among the team, enhance patient care, and help you identify improper billing practices and coding errors.
FAQs:
How do coding errors impact the billing process, and how can they be avoided?
Incorrect coding can lead to several problems, including fractional or delayed payments, increasing the claim processing timeline, instigating audits by the insurance company, and increasing the possibility of fraud charges. Coding errors can be avoided by training staff to stay updated with current coding requirements, ensure precise documentation, and improve staff collaboration.
What are some effective denial management strategies to prevent revenue loss?
By identifying core reasons for claim denials, implementing modern technology to address the issue of miscoding, training the staff to avoid billing errors, and regularly performing audits, you can minimize the risk of revenue loss in your healthcare facility.
How can advancements in technology and software improve billing accuracy?
Automating the coding process can minimize errors that would otherwise occur through manual coding, such as underbilling or overbilling. The use of technology such as electronic health records (EHRs) has significantly improved billing accuracy by streamlining data entry.
What is the role of medical billing audits in identifying and rectifying errors?
Medical billing audits include systematically reviewing coding and billing practices, which helps improve the accuracy of the billing process by ensuring compliance, correcting billing mistakes, and identifying any discrepancies.
Read More...9 Essential Medical Billing and Coding Tips for Healthcare Providers
Posted on July 28th, 2023 / Under Medical Billing / With No Comments
Medical billing and coding are complex procedures that play a vital role in ensuring accurate and timely reimbursement in the healthcare industry. Navigating the intricacies of these procedures and establishing the best practices to optimize revenue for the facility or practice is always a challenge for healthcare providers. Therefore, following these medical billing tips for doctors and clinics can help streamline the billing and coding processes.
1. Ensure Precise Documentation
One of the crucial medical billing best practices is to document with precision. Inaccurate documentation can lead to coding and billing errors that impact reimbursement levels.
Healthcare providers should document patient information precisely, avoiding any vague or incomplete details regarding diagnosis, services, procedures, and treatment plans.
This precise documentation not only facilitates the billing and coding process but also plays a crucial role in credentialing and contracting, expediting the verification of qualifications and allowing healthcare providers to discuss payment terms and rates with payers.
2. Stay Up-to-Date with Coding Guidelines
Staying informed of recent changes in CMS (Centers for Medicare and Medicaid Services) guidelines is essential, as CPT and ICD-10 medical codes undergo frequent updates.
Acknowledging these updates reduces coding errors, ensures no delays in reimbursement, and prevents claim rejections. Providing proper training to medical billing and coding staff, as well as other providers in the facility, regarding evolving coding guidelines is crucial to optimizing revenue.
3. Know the Importance of Compliance
Compliance is of utmost importance for medical billing and coding teams and healthcare providers.
Providers must have complete knowledge of all healthcare regulations, such as adhering to the HIPAA regulations, which impose severe legal repercussions on violators.
Prioritizing compliance and ethical procedures in medical billing and coding is essential for providers to avoid any legal repercussions.
4. Monitor Coding Accuracy
Implementing regular audits to assess coding accuracy within the facility is another best medical billing and coding practice. Regular audits help recognize any recurring patterns of coding errors that can influence reimbursement cycles, allowing appropriate corrective measures to be taken promptly. Addressing coding issues promptly minimizes compliance risk and reduces claim denials.
5. Promptly Submit Claims and Handle Appeals
Around 80% of all medical claims submitted to payers or insurance companies contain errors, leading to weeks’ worth of editing by medical billing and coding teams. These resubmissions cause delays in reimbursement.
Healthcare providers must ensure there is no missing or false patient and insurance information recorded, which could cause issues during the claims process. They must also file claims within given timelines and periodically review filed claims for consistency and accuracy, thus avoiding filing duplicate claims.
Reviewing claims helps identify common issues and potential areas of improvement, while being informed about appeal guidelines expedites the reimbursement process.
6. Streamline Communication
Encouraging open lines of communication between the billing and coding teams and healthcare providers is the first and foremost step to ensure a seamless billing process. Streamlining communication and collaboration among the teams within the healthcare facility fosters a workplace culture where misunderstandings and errors in billing and coding can be avoided by asking questions and clarifying doubts.
7. Leverage Technology
To streamline the billing and coding processes in your facility, leveraging technology and automation is crucial. Investing in medical billing software improves productivity and minimizes coding errors. For instance, integrating the EHR (Electronic Health Records) software with the medical billing systems makes scheduling appointments and submitting accurate claims more efficient.
8. Avoid Underpayments Through Payer Reimbursement Analysis
One main reason why most healthcare practices experience a loss of revenue is that they completely rely on the payer to reimburse them for the entire bill submitted. Payer discrepancies are fairly common in the industry, as each insurance provider or payer can have specific billing and coding requirements. Familiarizing yourself with each payer’s specific preferences regarding billing and coding increases the chances of maximizing reimbursement. Payer reimbursement analysis helps avoid under or overpayments.
9. Track Your Accounts Receivables
One main step to efficient revenue cycle management is to keep track of your accounts receivables, which are the outstanding payments owed to healthcare providers. Keeping track of these outstanding payments helps get timely reimbursement for the services rendered to patients.
FAQ
What Role Does Medical Coding Play In the Billing and Reimbursement Process?
Medical billing and coding play a vital role in translating complex medical procedures into standardized alphanumeric codes used to submit insurance claims for reimbursement of the services provided by healthcare professionals.
How Can Doctors and Clinics Handle Patient Billing Disputes Effectively?
Doctors and clinics can handle patient billing disputes effectively by verifying patient and insurance information, streamlining communication among the staff, issuing detailed invoices, and educating staff regarding current billing and coding trends.
What are Some Effective Patient Payment Strategies to Improve Collections?
Some strategies to improve collections include offering multiple payment options, integrating modern software for accurate billing, and training staff on collection techniques.
What Are Common Reasons for Claim Denials and How Can Clinics Reduce Them?
Common reasons for insurance claim denials include missing information, lack of medical necessity, and inaccurate coding. Clinics can reduce such denials through regular coding audits, recording accurate documentation, and promptly submitting claims.
What Are the Benefits of Using Medical Billing Software In a Clinic?
Medical billing software offers many benefits, including tracking outstanding payments, reducing coding errors, and speeding up claims submissions.
Read More...Unveiling the UB-04 Form: A Comprehensive Guide to Streamlining the Medical Billing Claims Process
Posted on July 11th, 2023 / Under Medical Billing / With No Comments
As a healthcare professional, you would be familiar with the importance of medical billing in optimizing a practice’s revenue cycle. Submitting claims and accurate billing can be complex and overwhelming procedures due to the ever-evolving insurance and compliance regulations- especially when you have to complete detailed forms like the UB 04 claim form.
Whether you are seeking a refresher or are new to the concept of medical billing, understanding what a UB 04 form is will assist you with streamlining the medical billing claims process as a healthcare provider. Keep reading to get a more practical insight and learn the fundamentals of the UB-04 claim form.
Overview of the UB-04 Form
Before we delve deeper into the preparation and completion of a UB-04 form, let’s first learn what is a UB 04 form used for and how to get a UB-04 form from the hospital. This will help you utilize the form in your medical billing practice.
Many people mix up the CMS-1500 form with the UB-04 claim form, but what the UB-04 form is used for is different from the purpose of the CMS-1500 form, which is physician billing. This is one reason why many medical billers get confused about when to use a UB-04 form and a CMS-1500 form.
The UB-04 form, formerly known as the CMS-1450, is a standard claim form used to bill healthcare claims for inpatient and outpatient services by an institutional facility.
Since its creation by The Centers for Medicare and Medicaid (CMS), the form has become widely popular in the healthcare industry and includes certain codes that insurance companies use. The UB-04 form generally contains detailed information on the patient, the provider, the services provided to the patient, and the total charge of the service, which would help you ensure accurate billing and receiving timely reimbursement for your services.
Understanding the UB 04 form used in what setting would also help you differentiate between UB 04 form and other forms used for billing purposes. Typically, UB-04 forms are used by institutional providers such as hospitals, hospices, health clinics and other healthcare facilities. By using the UB-04 form, you would not have to worry about completing and merging different forms together, cutting down the administrative burden for you.
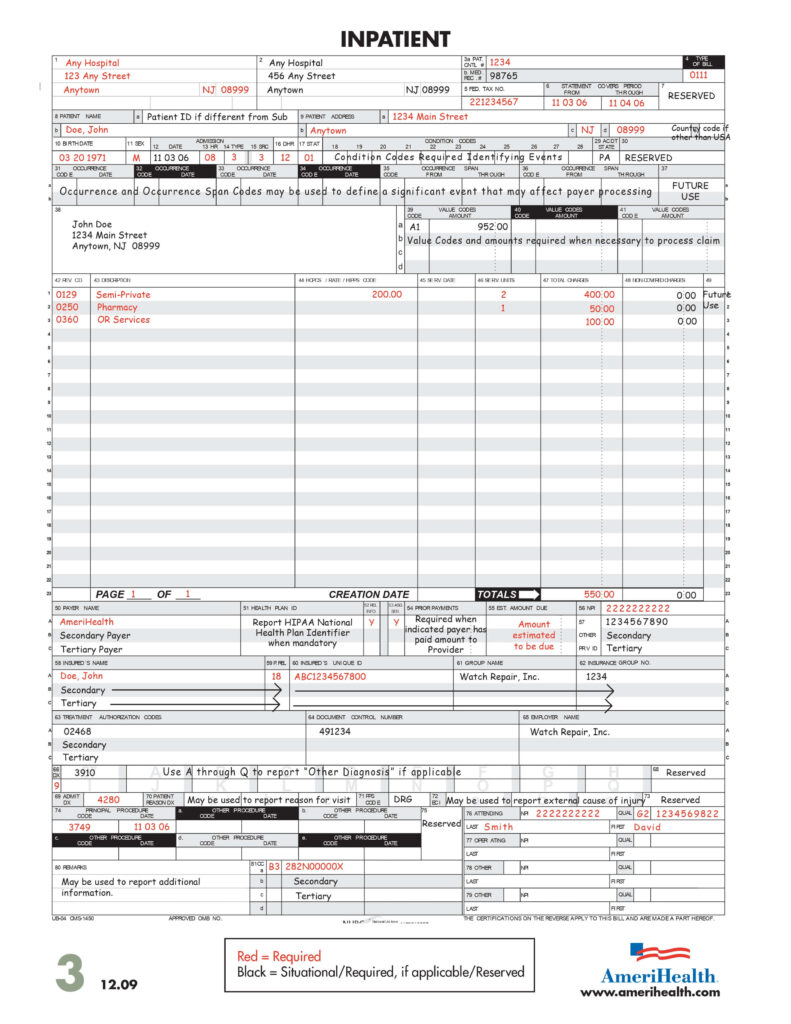
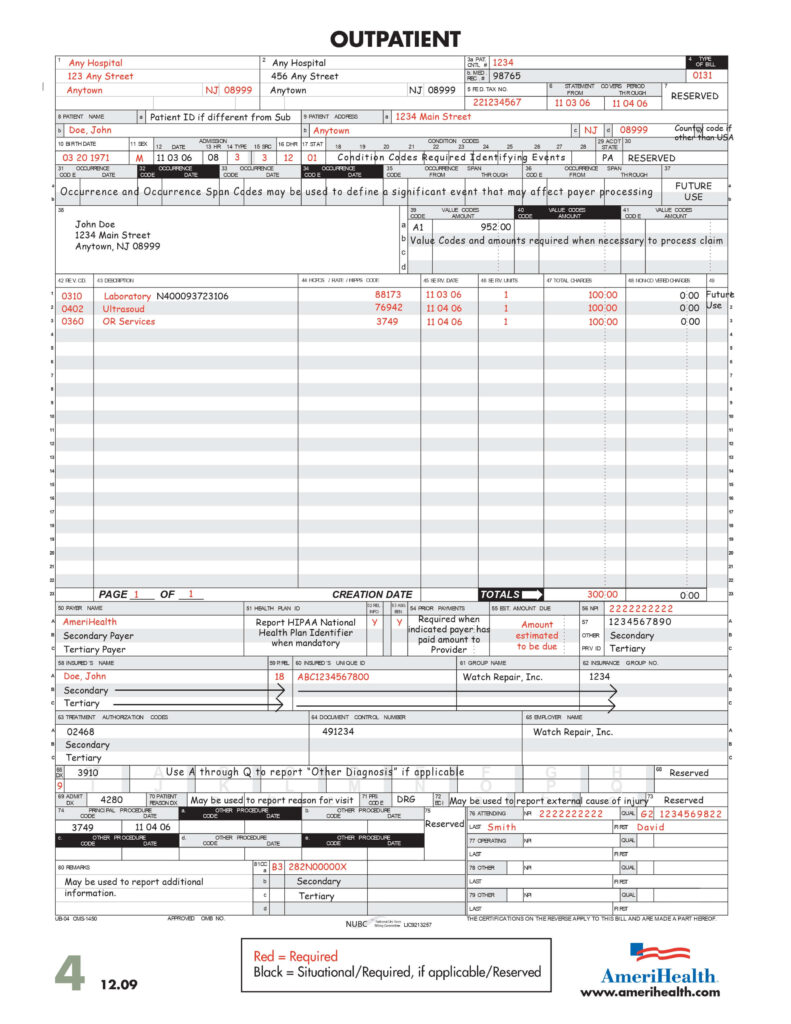
Source: https://www.amerihealth.com/pdfs/providers/npi/ub04_form.pdf
Preparing and Completing a UB-04 Form
The following are the UB-04 form instructions you should use when filling out a UB-04 form.
Collating Information and Contacting the Insurance Provider for Data Requirements
Before filling out the UB-04 form, you should collect all patient information, including their full name, date of birth, address, and insurance details. Adding the patient and provider information, including the provider’s National Provider Identifier, are crucial to completing the form.
There are around 81 UB-04 form fields, and specific sections on the UB-04 form indicate where the provider and patient information should be filled out. These fields are typically referred to as FL or form locators. You should know the specific purpose of each form locator to fill it when completing a UB-04 form correctly. Each field requires unique information, so after filling out the form, double-check the fields to ensure the information is accurate and there is no missing data.
You should also ensure to check in with each insurance provider to ascertain their specific data requirements for accurate form completion and billing. This helps you avoid any error that can lead to a claim rejection.
Identifying the UB 04 Type of Bill
The UB 04 type of bill code is used to identify the type of care and facility. For instance, it indicates whether the service is being billed as an inpatient, nursing facility, or outpatient. You should select the appropriate code and populate the form locator 4 (TOB) according to the UB-o4 form field descriptions.
UB-04 Codes List
Various codes are utilized in the UB-04 form to report billing information accurately. To understand these codes better, look at the UB04 type of bill codes list.
- Condition Codes: The form locations 18-28 on the UB-04 form are considered condition codes used to indicate the circumstances related to the bill that may affect its processing. For instance, codes related to the patient’s treatment or admission.
- Value Codes: Value codes are used to report the monetary value of an item or service. For example, value codes identify data such as days of treatment not covered by the primary payer and no-fault payments.
- Occurrence Codes: These codes describe specific events related to the claim. More than one occurrence code can be added depending on the circumstances surrounding the claim.
- Diagnosis Codes: Codes used to identify the patient’s reasoning for obtaining the healthcare service are known as diagnosis codes. These codes are typically added using the International Classification of Diseases or ICD coding system.
- Revenue Codes: Revenue codes are used in the UB-04 form to indicate the specific types of items and services provided to a patient during their stay at the healthcare facility.
- Procedure Codes: Healthcare Common Procedure Coding System (HCPCS) or Current Procedural Terminology (CPT) coding systems add procedure codes to the UB-04 form. These codes indicate the type of procedures or services performed.
It is important to list all these codes accurately in the form to collect reimbursement for the medical services provided to the patient. While these are only a few examples of the codes used in the form, you may have to deal with specific codes depending on the payer instructions and requirements, types of service, and healthcare facility. If a service is not properly coded, you can end up with rejected claims or delayed reimbursements.
Charges and Payments
When adding the total service cost, make sure you include any discounts and adjustments that will affect the total amount. This will ensure that the claims are paid properly.
Recording Dates and Submitting the Form
If the service provided is inpatient, you must add the admission and discharge dates. On the other hand, for outpatient services, you should add the start and end dates.
Once the form is completed, please adhere to the payer requirements and submit it either via mail or electronically. Ensure that you keep a copy of the form for record purposes.
Read More...
Recent Posts
-
False Claims Act Impact On Medical Billing and Coding
Initially, the False Claims Act in healthcare was enacted during the Civil wall to impose liability on individuals and organi...
Read More... -
Role of Encounter Forms in Provider Records and Billing
On average, a doctor wo...
Read More... -
Free Standing Emergency Rooms Billing Services And Your Need To Outsource
Freestanding ER may be a new trend in the healthcare industry, but they have been around for ages. The purpose of freestandin...
Read More... -
Physician Credentialing Importance In Healthcare Improvement
According to a recent survey, Read More...
-
Medicare 8 minute Rule Billing: Also Known As Direct Time CPT Codes
Underbilling is a serious issue in the healthcare industry, and one primary cause is the providers’ lack of knowledge regar...
Read More...
