Unveiling the UB-04 Form: A Comprehensive Guide to Streamlining the Medical Billing Claims Process
As a healthcare professional, you would be familiar with the importance of medical billing in optimizing a practice’s revenue cycle. Submitting claims and accurate billing can be complex and overwhelming procedures due to the ever-evolving insurance and compliance regulations- especially when you have to complete detailed forms like the UB 04 claim form.
Whether you are seeking a refresher or are new to the concept of medical billing, understanding what a UB 04 form is will assist you with streamlining the medical billing claims process as a healthcare provider. Keep reading to get a more practical insight and learn the fundamentals of the UB-04 claim form.
Overview of the UB-04 Form
Before we delve deeper into the preparation and completion of a UB-04 form, let’s first learn what is a UB 04 form used for and how to get a UB-04 form from the hospital. This will help you utilize the form in your medical billing practice.
Many people mix up the CMS-1500 form with the UB-04 claim form, but what the UB-04 form is used for is different from the purpose of the CMS-1500 form, which is physician billing. This is one reason why many medical billers get confused about when to use a UB-04 form and a CMS-1500 form.
The UB-04 form, formerly known as the CMS-1450, is a standard claim form used to bill healthcare claims for inpatient and outpatient services by an institutional facility.
Since its creation by The Centers for Medicare and Medicaid (CMS), the form has become widely popular in the healthcare industry and includes certain codes that insurance companies use. The UB-04 form generally contains detailed information on the patient, the provider, the services provided to the patient, and the total charge of the service, which would help you ensure accurate billing and receiving timely reimbursement for your services.
Understanding the UB 04 form used in what setting would also help you differentiate between UB 04 form and other forms used for billing purposes. Typically, UB-04 forms are used by institutional providers such as hospitals, hospices, health clinics and other healthcare facilities. By using the UB-04 form, you would not have to worry about completing and merging different forms together, cutting down the administrative burden for you.
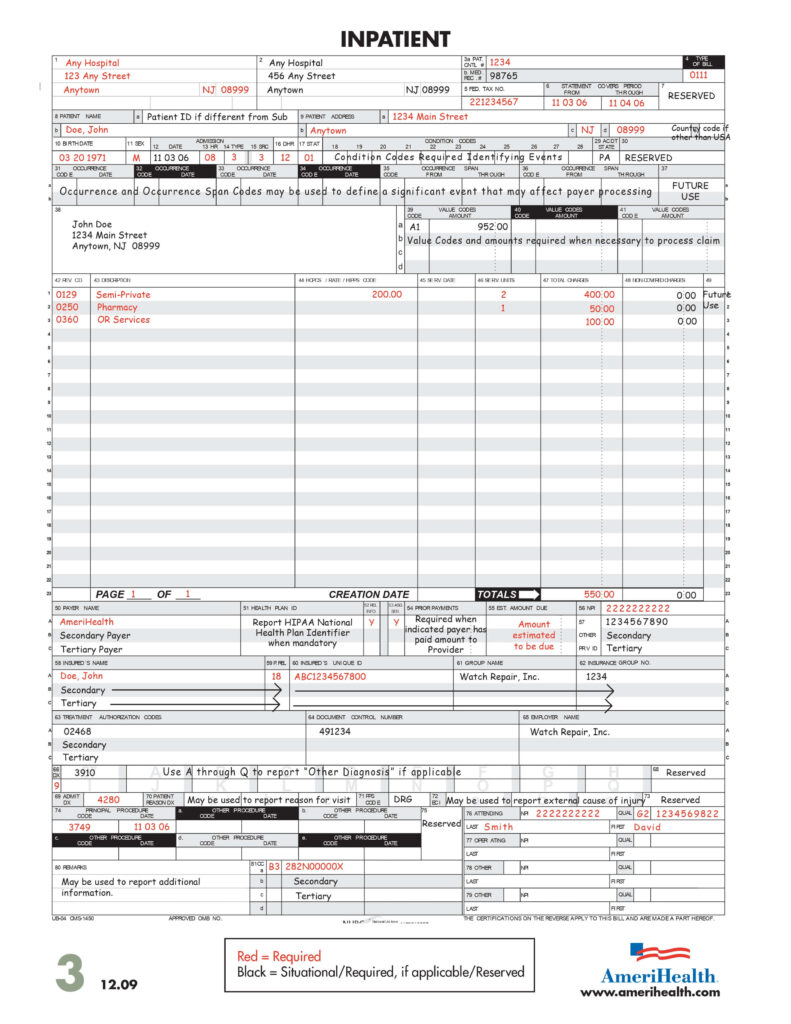
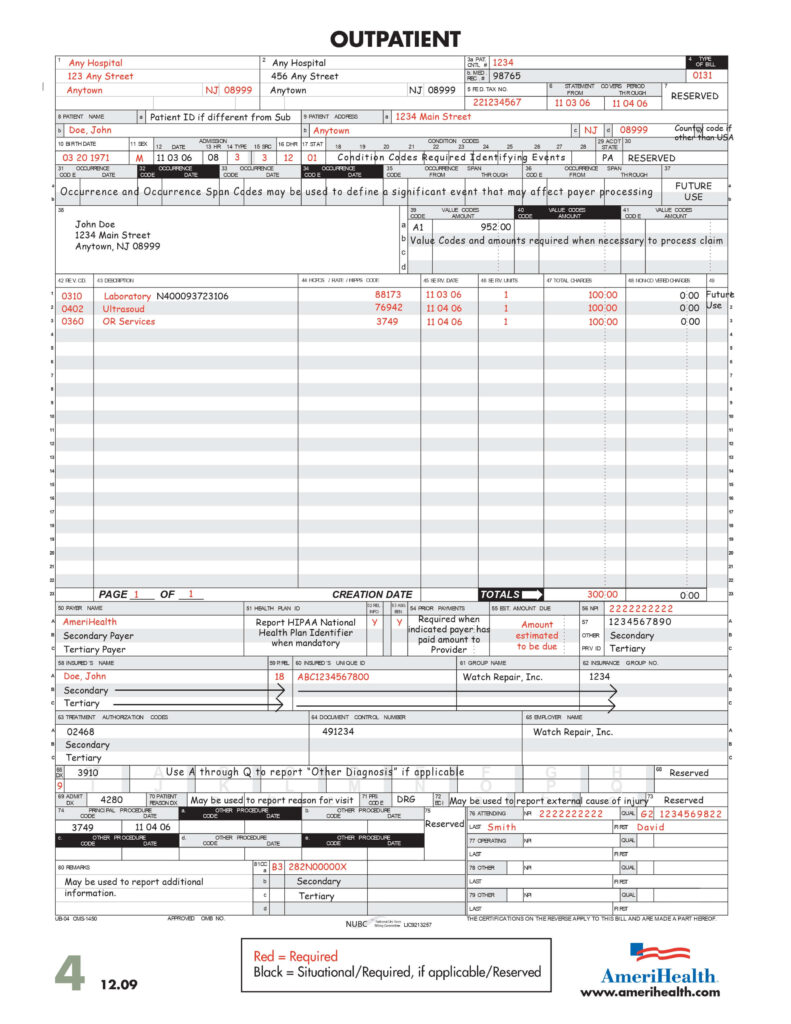
Source: https://www.amerihealth.com/pdfs/providers/npi/ub04_form.pdf
Preparing and Completing a UB-04 Form
The following are the UB-04 form instructions you should use when filling out a UB-04 form.
Collating Information and Contacting the Insurance Provider for Data Requirements
Before filling out the UB-04 form, you should collect all patient information, including their full name, date of birth, address, and insurance details. Adding the patient and provider information, including the provider’s National Provider Identifier, are crucial to completing the form.
There are around 81 UB-04 form fields, and specific sections on the UB-04 form indicate where the provider and patient information should be filled out. These fields are typically referred to as FL or form locators. You should know the specific purpose of each form locator to fill it when completing a UB-04 form correctly. Each field requires unique information, so after filling out the form, double-check the fields to ensure the information is accurate and there is no missing data.
You should also ensure to check in with each insurance provider to ascertain their specific data requirements for accurate form completion and billing. This helps you avoid any error that can lead to a claim rejection.
Identifying the UB 04 Type of Bill
The UB 04 type of bill code is used to identify the type of care and facility. For instance, it indicates whether the service is being billed as an inpatient, nursing facility, or outpatient. You should select the appropriate code and populate the form locator 4 (TOB) according to the UB-o4 form field descriptions.
UB-04 Codes List
Various codes are utilized in the UB-04 form to report billing information accurately. To understand these codes better, look at the UB04 type of bill codes list.
- Condition Codes: The form locations 18-28 on the UB-04 form are considered condition codes used to indicate the circumstances related to the bill that may affect its processing. For instance, codes related to the patient’s treatment or admission.
- Value Codes: Value codes are used to report the monetary value of an item or service. For example, value codes identify data such as days of treatment not covered by the primary payer and no-fault payments.
- Occurrence Codes: These codes describe specific events related to the claim. More than one occurrence code can be added depending on the circumstances surrounding the claim.
- Diagnosis Codes: Codes used to identify the patient’s reasoning for obtaining the healthcare service are known as diagnosis codes. These codes are typically added using the International Classification of Diseases or ICD coding system.
- Revenue Codes: Revenue codes are used in the UB-04 form to indicate the specific types of items and services provided to a patient during their stay at the healthcare facility.
- Procedure Codes: Healthcare Common Procedure Coding System (HCPCS) or Current Procedural Terminology (CPT) coding systems add procedure codes to the UB-04 form. These codes indicate the type of procedures or services performed.
It is important to list all these codes accurately in the form to collect reimbursement for the medical services provided to the patient. While these are only a few examples of the codes used in the form, you may have to deal with specific codes depending on the payer instructions and requirements, types of service, and healthcare facility. If a service is not properly coded, you can end up with rejected claims or delayed reimbursements.
Charges and Payments
When adding the total service cost, make sure you include any discounts and adjustments that will affect the total amount. This will ensure that the claims are paid properly.
Recording Dates and Submitting the Form
If the service provided is inpatient, you must add the admission and discharge dates. On the other hand, for outpatient services, you should add the start and end dates.
Once the form is completed, please adhere to the payer requirements and submit it either via mail or electronically. Ensure that you keep a copy of the form for record purposes.
