On average, a doctor works around 51.4 hours a week, seeing around 11-20 patients a day. With these numbers, it’s challenging...
- Welcome to One Source Medical Billing
- 888-624-5563
- [email protected]
- 6810 N. State Road 7 Coconut Creek, FL 33073

Underbilling is a serious issue in the healthcare industry, and one primary cause is the providers’ lack of knowledge regarding Medicare rules. One commonly understudied Medicare rule is the 8 minute rule.
At first glance, the Medicare 8 minute rule seems fairly straightforward; treatments are billed to Medicare in units, and treatment must last no less than 8 minutes for a unit to be billed to Medicare.
Unfortunately, oversight in this regard could lead to mistakes, resulting in problems like incorrect billing, underpayment, or delayed reimbursement.
As a provider, here is how to avoid mistakes when using the 8 minute rule units to bill Medicare.
As established earlier, to receive payment from Medicare for some CPT codes, a provider should provide direct treatment to a patient for a minimum of 8 minutes.
Any service, specifically outpatient therapy services like physical or occupational therapy, that lasts less than 8 minutes in duration, cannot be billed to Medicare. This rule also only applies to time-based CPT codes.
It’s also crucial to understand that only certain services fall under this rule, such as Medicare Part B services. It also applies to payers who follow Medicare billing guidelines; in addition, the 8-minute rule only applies when the service is performed in person.
Services covered by the Medicare 8 minute rule are billed in 15 units.
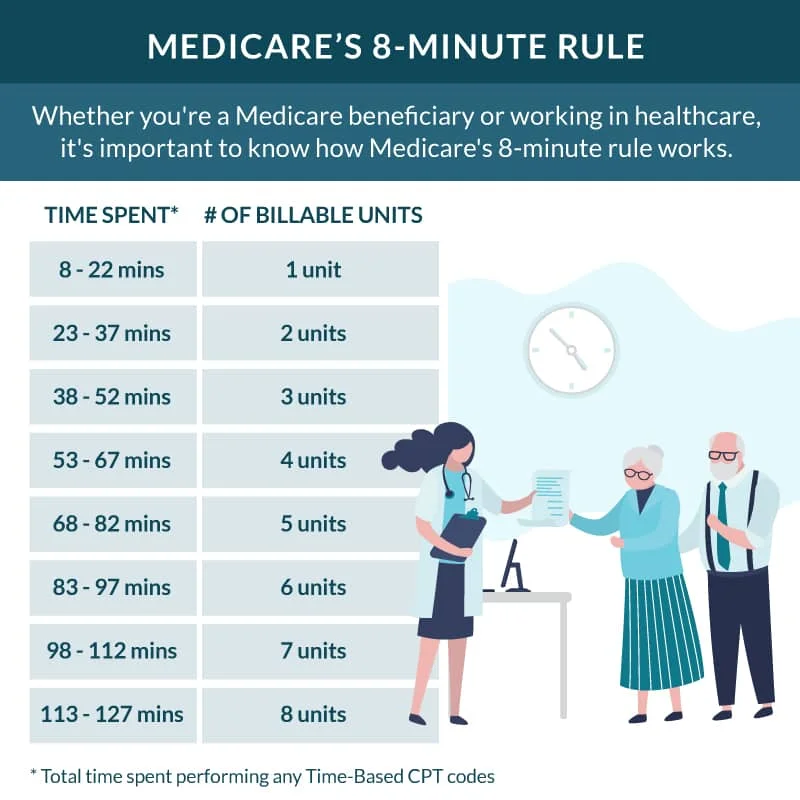
For example, if a service lasts anywhere between 8 to 22 minutes, it would be billed in a single unit. But if the service takes more than 22 minutes, such as 37 minutes, Medicare will be billed 2 units for each 15-minute interval and so on. You can review the Medicare 8 minute rule chart for a clear understanding of billable units.
However, any services that last less than 8 minutes may not be separately billable. In case a patient is provided more than one service or procedure in a single minute, Medicare would review the combined minutes of each service. If the combined minutes pass the minimum threshold of 8 minutes, Medicare can be billed separately for each type of service.
The CMS 8 minute rule applies to outpatient service providers, including hospital outpatient departments, private physical therapy clinics, rehabilitation facilities, occupational therapy clinics, nursing facilities, and speech-language pathology centers.
Medicare rules, such as the AMA 8 minute rule, do not apply to non-medical insurance unless stated explicitly in their policies. That is because most private insurance companies don’t allow mixed remainders.
Mixed remainders are referred to as the leftover hours of a multiple-timed service that do not meet the minimum threshold. Mixed remainders from different services can be combined to meet the 8-minute threshold and be billed as units. Moreover, the 8-minute rule also applied to Medicaid services.
You can also refer to the 8 minute rule cheat sheet to understand the difference between billing for insurances that follow CMS guidelines and those that follow AMA guidelines.
Service-based codes are generally untimed and billed as a single unit as they do not depend on the amount of time a service takes. Some common examples of service-based codes are E/M (Evaluation and Management) codes, procedures, and diagnostic tests. Service-based codes are reimbursed depending on the complexity of the service provided.
On the other hand, time-based codes are billed in 115 increments, depending on the amount of time spent on a service. There is also a set of rules that apply to make time-based codes billable. For example, the service provided should have been one-on-one for a time-based code to be reimbursed.
In some cases, time-based units and service-based units can be a part of the same treatment session, but they will still be billed separately.
Knowing how to calculate medical billing units is essential for claims scrubbing and submission. Here is how you can calculate billable units.
Consider this example: if the total number of minutes you spent on a time-based service was 30, you can divide it by 15. This way, you will get two billable units.
Many people confuse the rule of 8s with the Medicare 8 minute rule when, in fact, the rule of 8s is the label used to describe the 8 minute rule in the CPT code manual. Typically, the rule of 8s is applied to non-medical insurance payers for Direct Time CPT Codes.
While the rule of 8s follows the same principles as the 8-minute rule, there is a bit of distinction. For instance, the rule of 8s requires practitioners to provide at least half of the service to bill for one unit.
It can be challenging to properly bill under the Medicare 8 minute rule for physical therapy.
There are often certain mistakes people make, like presuming they’ll be getting charged extra for services lasting longer than 8 minutes or believing that this rule applies to all types of services provided by their assigned physician.
Physicians should discuss the 8 minute rule with Medicare beneficiaries to alleviate their concerns and answer relevant queries.
On the provider end, to avoid any billing mistakes while using the 8 minute rule, you should,
How many minutes are in a billing unit?
According to the 8-minute rule by Medicare, a billing unit typically equals 8 minutes of a physician’s time. So, if a physician performs a service that takes around 8 minutes, it will be billed as one unit.
8-minute rule importance in physical therapy?
The 8 minute rule guides physical therapy specialists on how to properly document their time during a patient encounter and perform accurate billing for reimbursement. Adhering to the 8 minute rule helps physical therapy clinics optimize revenue.